from The Frontline
Tampa, Florida, US
Unsettled Units !
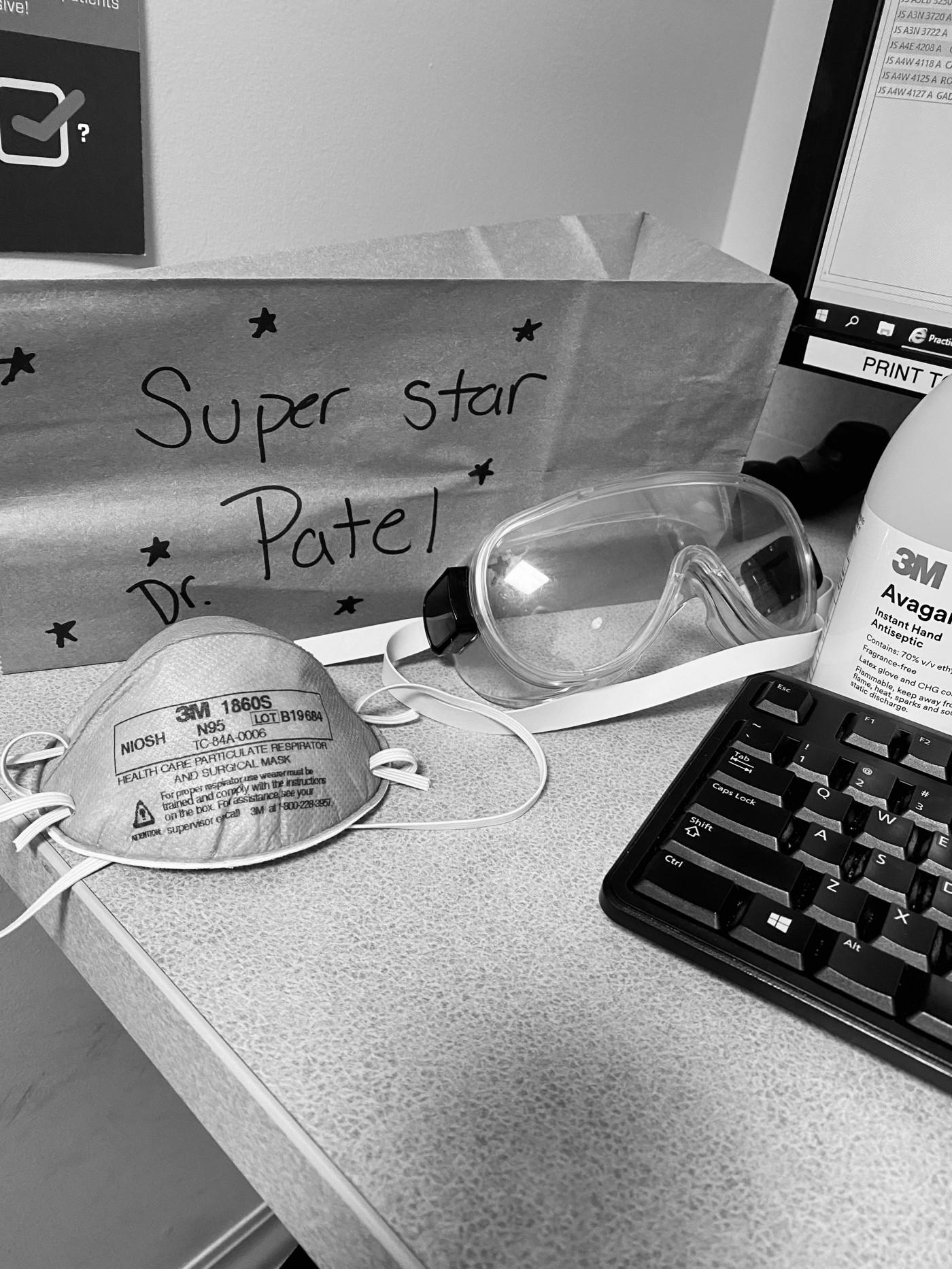
I usually wake up around 530 am. There has been sense of uneasiness in our home for last few days. It is like everyone knows something and no one wants to talk about it. Even though I was working weekend prior, I was able to come home by 5 pm, we call it easy day. News about climbing death toll in Italy is all over at this point. Images has been of nothing but horror. There has been impatient peace in house, we have two teenagers in house. So, restlessness and curiosity are our nature. Things which we cannot control always makes us more anxious more so, in world which seems ever unpredictable and at times threatening. When you are left to fend for yourself after putting all trust in society which we collective inhabit and network of safety net becomes illusion, future somehow is rattled. Eutopia has eluded humanity since eons. So, when I shaved my face that Sunday evening it became an event. We all laughed at my clean shaved face. Little everyone knew mask only fits well on shaven face. N-95 mask or respirator has its own character. It needs to hug tightly to your face for it to work. 95 % efficacy in removing micro particles depends upon seal of the mask to your face. I have been mask fitted few days prior. Even when you pass test, you never feel completely comfortable about those fit-tests. Because mask is only thing could potential prevent you from dying. One .06 microns of deadly virus is all it takes to go between mask and your face. And it could kill you. Times have changed. Walking around without masks some how feels like walking around naked! Fresh mask smells like
I arrive at hospital 700. I am a critical care physician. We are specially trained physicians to take care patients in ICU. It is specialty that requires on and average 6 years of harsh training after medical school. We are not your heart doctors or kidney doctors. But we are there to hold onto life when everything fails. We live with death and fight for life. Somehow try to bribe God to bend destiny. Out job is not glamorous, it is full of smell of blood and more. Critical care physicians or intensivists are new phenomenon in ever complicated American health care system. Advent of complex interventions to sustain life and support sophisticated surgery enabled by modern technological advancement created need for Intensive Care Units in all hospitals. It started becoming ubiquitous in all hospitals after widespread use or coronary interventions for cardiac patients after coronary artery disease epidemic in mid 1980s. Initially any physicians can manage patients in ICUs. But as life-sustaining technology became more advanced it needed highly trained doctors and nurses to manage that complicated pathophysiology and manage interface between humans and ever evolving high tech machines. Human life in ICU is always has been homo dueos as in ‘Sapiens’, conglomeration of humans and machines to defeat Darwanian evolutions. Every life matters. As medicine became more ambitious and technology became more sophisticated, our interventions also became more audacious. That needed more beds in hospital to cater those critically ill patients. As Americans are getting older there has been a demographic volcano bubbling under calm and collective illusive homogeny of efficient system. Our health care started overrun by bureaucrats and managers and it lost vision for strategic planning in name of efficiency. On average you will need 10 % beds in hospital which could be ICUs. But caring for those patients are expensive and exhaustive. Mortality of those patients ranges around 10% and could very, length of hospital stay could be in weeks and cost hundreds of thousands. So, there is no strategic pile of these beds, and there are no providers who have been strategically piled somewhere. It is all us. It is all you get. And it stops there.
It is second week of March; we have been preparing. Or pretend to prepare. I had to cancel our family Portugal trip for spring break few days back with some eerie anticipation. Not that I was afraid, but If I get quarantined for two weeks, it will be difficult for my partners to carry on if there is sharp uptake in critically ill patients. And now I am considered strategic asset for state. Florida is hot bed of human frailty. We always have been vulnerable and usually unprepared at best. Even small-scale hurricanes have proven challenging at times. So, predictably our leaders and population has been unprepared, slow and eccentric. Ever changing guidance from CDC and WHO did nothing to calm our nerves. With evolution of managed health care, it has been clear to us that we, as a provider are providers are the ones that needs to be managed. So, we wait for our managers to decide fate of our patients and ultimately ours. So, one day we will wear surgical mask for COVID-19 patient, next day we will need respirator, other day we will need to reuse respirator and day after we will wear surgical mask on top of respirator. Once you get exposed to virus, guidance changes every day. You could be quarantined, tested, watched, treated or nothing at all. Hospital Administrators will hide behind that guidance and dictate your life and may be death.
I go to computer station and print my patient list and looked for sign-out from previous provider. Respiratory therapist hurried in office with arterial blood gas values. Respiratory therapists are totally unsung heroes in COVID-19 pandemic. These are technicians trained to help nurses and physicians to take care or breathing problems for their patients. They do everything from helping collect phlegm specimen, giving breathing treatments to patients in respiratory distress to managing ventilators. These are the experts who will covert one ventilator serving into two patients or use sleep apnea devices as makeshift ventilators. As this virus gets transmitted by airborne particles, they are the front lines and exposes themselves to virus more than any other professionals. Blood gas was decent, somewhat low oxygen and normal carbon dioxide. This would have been normal in our ICU. But his patient was in PCU, which is progressive care unit. A kind of stepdown units for patient who does not require high degree of intensive care. So, I ask how much oxygen he is on? That is standard question. That helps us to determine how much oxygen patient needs to maintain current blood oxygen. If patient is requiring too high oxygen that would be bad sign, meaning lungs are not working properly. This patient was on 70 % oxygen on BiPAP and struggling. BiPAP is positive pressure device which pushes oxygen via pressure through mask sealed over nose and mouth. This usually is used to prevent patient from needing to be placed on ventilator while we wait for medications to work and patients to improve. This device has saved lots of lives and reduced length of stay in ICUs dramatically. Main problem patients have is hard time keeping mask on the face and air usually leaks around mask.
“ He has been admitted with respiratory failure with COVID-19 rule out, doctor”. I jumped off my chair. On BiPAP ? By now we know this disease spreads by respiratory droplets. BiPAP mode of respiratory support is notorious for making these droplets spread worse. As patient breaths or coughs out against pressure supported by BiPAP, it gives boost to velocity of this droplets. So, every time patient exhales or coughs particles spreads further making more people in its range. This is hot zone magnified. We know this virus is very infectious, anyone who gets exposed will very likely be infected. So, apparently patient was admitted night before with respiratory distress and currently on BiPAP, it exposed everyone who took care of him throughout night. This would be a nightmare scenario. If this would not have been COVID-19 patient, BiPAP would have been fine, but I had to make a split-second decision to intubate this patient. Intubation means putting breathing tube down trachea so we can manage breathing through machines.
These are the unsettling moments. This is our moment. This patient needed to be admitted in negative pressure rooms, where air in room can circulate at faster pace filtering viruses through specialize air filter. This was not that room. If we transport this patient to other room, there was risk of contaminating hallway and putting other providers at risk. We decided to do procedure in original room for safety of others. You put your gown and gloves. Put your mask best you can, every second counts. But every single mistake could threaten life, either yours or patients. Thousands of thoughts come to your mind. Your kids, family, your memories. Your struggles and unfinished living will, now suddenly matters more acutely than ever. Your heart races than stops. “Whole life of the individual is giving birth to himself, indeed, we are fully born when we die”. Intubating someone takes only few seconds, but unplanned intubations could be catastrophic. Intubations in these patients are like you just entered full on virus shower with your masks, gloves and gown. You only hope you will not get wet. And if you get, it might kill you. When I walked in his room, patient was alert and aware. He was dazed and his eyes looks starry. He was scared and uncontrollably coughing and in distress. I explained procedure and he begged to talk to his wife, see his kids. At this point families are not allowed in hospital and arranging for videocall would require too much time for his own safety. So, he agreed that I would call his wife as soon as we put him to sleep. At that moment we both knew I could be last person talking to him before he dies. Somehow saddest part of doing my job is seeking patients dying lonely..by themselves. Consciousness is always beyond something science has not been able to explore or explain. I believe in eastern philosophy of collective consciousness. May be when we die, consciousness merges into universal singularity. Dying alone just feels like denying passage of that consciousness to its own destiny. Somehow you get it done. Move patient to ICU. And then start doubting yourself. Was mask fitted right? Was my neck still exposed? Did I touch my face after that? Did I take gloves and mask off in right sequence? Doffing is what we call removing your garb. That is when providers most likely get infected. May be out of complacency. Then you realize you don’t have time to think about yourself. This patient needs more care. Since this patient had very low oxygen level even after adjusting for higher pressures, and rapidly deteriorating condition, we decide to prone patient. Somehow these patients with respiratory distress are doing well when they are placed on their chest, it improves oxygenation and cardiac function. As could be imagined, this is labor intensive procedures, but our wonderful nurses are always up for the challenges and got it done.
After patient stabilizes, I called his family. Talking to families of sick patients is more daunting than taking care of patients. This becomes entirely nerve raking when families can not be there with their loved ones. Looking into someone’s eyes bring different perspective to any communication. Without that it more difficult to justify anything you will be saying. Still you must try your best to make a case for better outcomes, that too against all odds. That is what critical care doctors do. Have hopes in fragility of life and futility of times. We are day dreamers; we are the ones who gets caught between life and death. We must justify death at cost of life for our own peace of mind. And move on to next patient and do all over again. No, wonder we are perennial stressed as subspecialty. Work is hard and rewards are far and few. So, current shortage of intensivists has something in making for long time. Poor working environment, inadequate pay scale and shortsighted leaders have created this vacuum. You cannot train these skilled physicians in one year. It will require herculean will to correct inadequacy in American Health Care, and that too, will take years to fix pasts mistakes. We never wanted to be in headlines until we became emergency room for hospitalized patients! One ventilator at a time. We will be managing those hundreds of thousands of ventilators after society moves on to different priorities. These patients will need same care for weeks and months for them to recover. Stakes will be higher even after surge abates. We will be the ones who will be taking patient off ventilators. We will be waking up in middle on night to investigate those ailing lungs, we are going to be there when patient gains consciousness. We will be putting ourselves again on harms way and too willingly. We will pave a road of comfort when letting them die in peace once their pain is inconsolable and everything fails. But for now we need someone to hold our hand, look in to eyes and lend us comfort we are so expertly providing to patients.
We will call him Mr.S. 62year old otherwise healthy. He has wife and two children. He went to New Orleans to bring back his ailing mother in law. His wife went with him. They came back 10 days ago. He had been having mild cough and fever. For last 24hrs breathing was getting worse and getting much weaker. I realized his 84year old mother in law was also in sister hospital with respiratory failure. I rushed to call my colleague that mother in law should be treated as COVID-19 patients under investigation. Ironically called PUI. Sooner I realized she died of respiratory failure soon after. These are unsettling times in ICUs. How can you talk to Mrs S. about her husband whose mother just passed? It is just not fair. I made a point to call his family every day. They were nice and gracious. I would imagine kids were in 30s. We did good job keeping Mr S. alive for 12 days now. He is still on ventilator. And family forever anxious and righteously impatient. How do we explain each passing day, chances of meaningful recovery becomes smaller and smaller, while family’s hopes and expectation keeps on going higher and higher?
We live in world with few answers. In my opinion we just make up answers to justify our shortsighted narratives. We all were expected to lead and leave world better than what we found. Working in critical care brings these notions in challenge every day. When air becomes poison nothing else matters in life. What we have, what we want and where are we going needs to be reflected in our civic conversations. Until then some of us will be coming home contaminated, trying to distance our kids and sleeping alone with hopes that it will prevent from passing those maladies to our loved ones. World owe us for that and will remain unsettled until.